Eligibility Verification Without the Overhead
Real-time eligibility in your PMS. Zero manual payer interactions. Zero disruption. Needletail fixes your margins
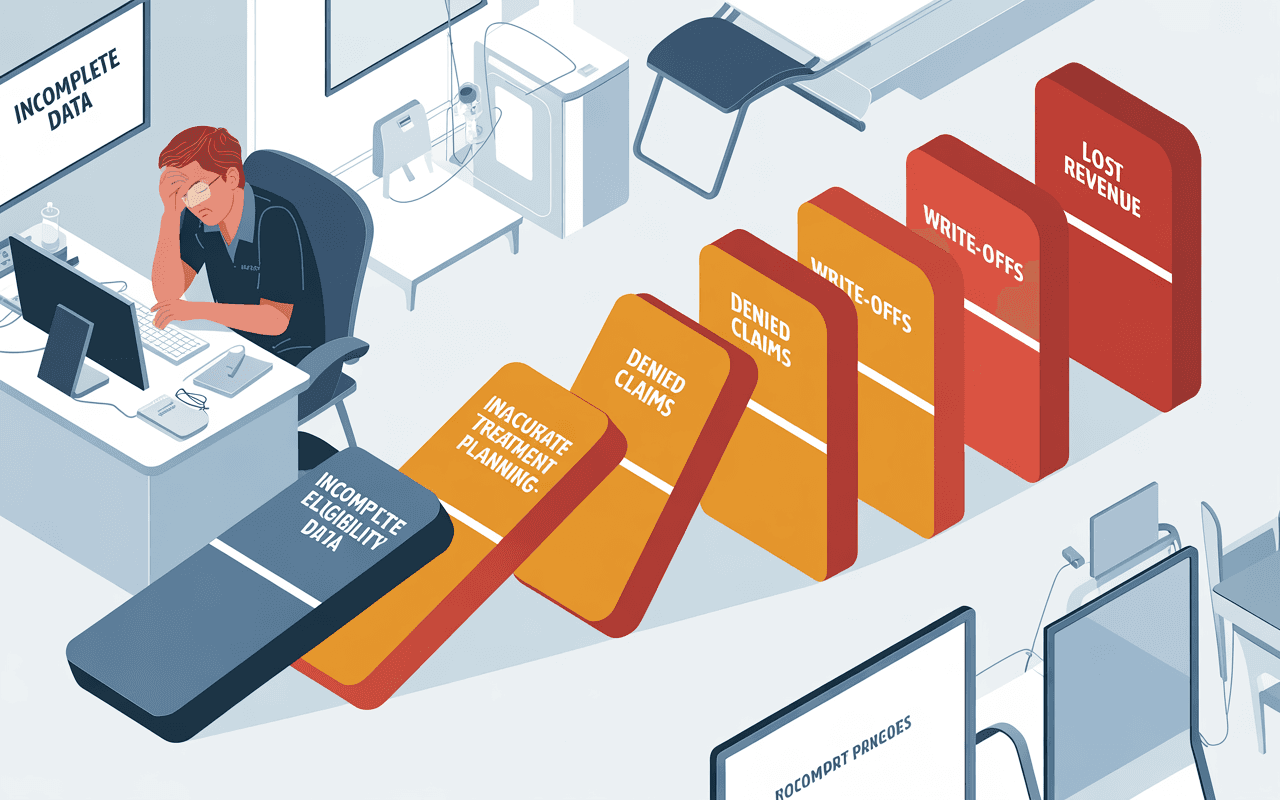
Manual eligibility is killing your margins
Hours wasted verifying benefits means less time for patient care—and lost revenue.
Hours lost to payer portals
Your team logs into multiple insurance portals daily, waits on hold with IVRs, then manually re-enters data into your dental PMS.
Treatment plans built on bad data
Incomplete or outdated eligibility info leads to inaccurate estimates, denied claims after treatment, and write-offs.
Patient sticker shock at checkout
Manual verification errors mean patients get surprise bills after their appointment—eroding trust and making collections harder.
Wasted on manual payer portals, IVRs, and spreadsheet
Due to incomplete eligibility data
Cost of eligibility-related denials and write-offs
Fully-loaded cost of manual verification
How Needletail Eligibility Verification works
AI + human verification. Speed without sacrifice.
Parallel AI Agents
AI logs into payer portals and calls IVRs simultaneously. Pulls live benefits data in seconds, not minutes.
Continuous QA
Cross-checks data, learns payer rules, flags edge cases. Gets smarter with every verification.
Specialist Review
Dental RCM specialists review flagged cases. Correct interpretation, compliance logged, full audit trail.
Verified eligibility in your PMS
Ready to transform your Eligibility & Benefits Verification?
You keep operating as usual while Needletail moves eligibility into autopilot.
Schedule Your 20-Minute Strategy CallWhy Needletail Eligibility & Benefits Verification is different
Built for group practices and DSOs that are done with manual eligibility.
SWIFT
Scalable
AI agents handle eligibility across 5 or 50 locations in parallel. Scale practices, not headcount.
Workflow-Native
Lives inside your PMS. No new tools to learn. Eligibility data just appears in patient records.
Implementation Speed
From signature to live eligibility in 10 working days. Zero downtime, parallel rollout.
Full Coverage
100+ US dental carriers. Portal and voice verification. Coverage for your real payer mix.
Trusted Partnership
Dedicated account manager. 24/7 support. AI backed by humans who understand dental RCM.
Better cash flow, zero surprises
What eligibility done right unlocks for your business
Perfect Eligibility Visibility
Your team knows exact coverage, copays, deductibles before treatment planning begins. Estimates are accurate. Case acceptance improves.
Minimized Denials
Eligibility-related denials drop 50%+. Claims submit clean. Fewer appeals. Faster reimbursement.
Improved Patient Experience
Patients know costs upfront. No surprises at checkout. Trust increases. Collections get easier.
Enhanced Cash Flow
Faster claim processing. Fewer write-offs. Better payment planning downstream. RCM operates like clockwork.
The Downstream Effect
This is how you build a revenue cycle that works for you, not against you.
Common questions about Needletail EBV
Still fighting eligibility fires
or ready to stop?
See how Needletail verifies tomorrow's patients before your team clocks in

